Understanding and Addressing Suicide Risk in Bipolar Disorder
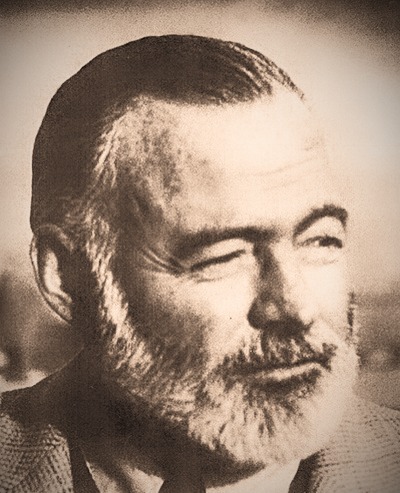
This Nobel Prize-winning author was prone to manic-depressive behavior throughout his life, a family trait shared by his parents, his son, and his granddaughter Margaux. Despite his larger-than-life personality and novels like A Farewell to Arms and For Whom The Bell Tolls, Hemingway had bouts of depression and paranoia. Obsessed with death, he eventually shot himself in 1961.
https://pubmed.ncbi.nlm.nih.gov/17326729/
Bipolar Disorder & Suicide:
The Critical Reality We Must Address
Bipolar disorder carries one of the highest suicide risks among all psychiatric conditions, a sobering reality that demands our collective attention and action. Recent comprehensive research reveals that individuals with bipolar disorder face suicide rates approximately 10 to 30 times higher than the general population. To put this in perspective, between 6% and 20% of people with bipolar disorder die by suicide, while 23% to 34% attempt suicide at least once during their lifetime.
These statistics represent real people—our colleagues, friends, family members, and community members. Understanding the risk factors and available interventions can literally save lives.
Recognizing the Most Vulnerable Moments
The research tells us that suicide risk in bipolar disorder is not constant—it peaks during specific mood states and life circumstances. Contrary to what many might assume, the highest risk occurs not during manic episodes, but during depressive and mixed states. These periods of profound despair, often combined with the agitation of mixed features, create particularly dangerous windows of vulnerability.
Age plays a crucial role in vulnerability patterns. Young adults under 30 to 35 years old show the highest relative risk compared to their peers without bipolar disorder. A second peak emerges in those over 75 years old. For children and adolescents with bipolar disorder, the risk increases progressively through adolescence, reaching alarming levels in older teenagers. This knowledge helps us understand when extra vigilance and support are most critical.
The Compounding Effect of Co-occurring Conditions
The presence of additional psychiatric conditions dramatically amplifies suicide risk in bipolar disorder. Three categories of comorbidities stand out as particularly concerning:
Anxiety disorders frequently accompany bipolar disorder and independently elevate suicide risk, especially when occurring alongside depressive or mixed episodes. The combination creates a perfect storm of emotional distress and hopelessness.
Substance use disorders nearly double the odds of suicide attempts in people with bipolar disorder. Alcohol use disorder, the most prevalent comorbidity, shows particularly strong associations with both suicide attempts and completed suicides. The presence of both alcohol and drug use disorders can create a multiplicative effect on risk. These substances exacerbate impulsivity, aggression, and mood instability—all established risk factors for suicidal behavior.
Borderline personality disorder emerges as a particularly strong predictor of suicidal behavior, including violent suicide attempts, in individuals with bipolar disorder. This combination reflects greater illness severity and psychosocial dysfunction that compounds overall risk.
Additional factors that elevate risk include male sex, living alone, divorce, unemployment, rapid cycling patterns, impulsivity, and comorbid medical conditions. The first year after hospital discharge represents an especially high-risk period requiring intensive support and monitoring.
The Critical Risk of Antidepressant Monotherapy
A crucial but often overlooked factor in bipolar suicide prevention involves the paradoxical danger of standard antidepressant medications. While antidepressants are essential for treating unipolar depression, using them even with mood stabilizers in bipolar disorder can trigger manic, hypomanic, or mixed episodes—precisely the mood states where suicide risk peaks. These medication-induced "switches" are particularly dangerous when they create mixed states, combining the hopelessness of depression with the energy and impulsivity of mania. Research shows this can double or triple mood episode frequency, destabilizing the illness and significantly elevating suicide risk over time.
This understanding fundamentally shapes evidence-based treatment. Rather than reaching for antidepressants when bipolar depression strikes, modern protocols prioritize mood stabilizers like lithium, lamotrigine, or certain atypical antipsychotics that address depression without triggering dangerous mood switches. When antidepressants must be considered, they should only be used alongside robust mood stabilization and careful monitoring. Avoiding antidepressant monotherapy and even combination therapy represents a critical safety measure that can literally mean the difference between life and death.
Evidence-Based Interventions That Save Lives
The Unique Role of Lithium
Among all available treatments, lithium stands alone with consistent, strong evidence for reducing suicide risk in bipolar disorder. Research demonstrates that lithium reduces suicide mortality a reduction of 60% to 67%. This antisuicidal effect appears unique to lithium and extends even to patients with comorbid psychiatric conditions.
While other mood stabilizers like valproate show some protective effects, they don't match lithium's antisuicidal profile. Lamotrigine effectively treats bipolar depression but shows less evidence for suicide prevention. Atypical antipsychotics help manage acute symptoms but demonstrate less clear impact on suicide risk.
The Power of Psychological Interventions
Psychological treatments play a vital complementary role to medication in suicide prevention. Three approaches show particular promise:
Psychoeducation helps individuals and families understand bipolar disorder, recognize warning signs, and improve medication adherence. By stabilizing the illness and improving engagement with care, psychoeducation indirectly reduces suicide risk. This intervention can be delivered individually, in groups, or with family involvement.
Cognitive Behavioral Therapy (CBT) directly targets the negative thinking patterns and hopelessness that fuel suicidal ideation. Meta-analyses demonstrate that CBT reduces both depressive symptoms and suicidal thoughts in people with bipolar disorder. The therapy helps individuals develop coping strategies and challenge distorted thinking that can lead to suicidal crises.
Dialectical Behavior Therapy (DBT) proves especially effective for individuals with high emotional dysregulation, including those with comorbid borderline personality disorder. Recent randomized trials show DBT reduces suicide attempts in both adolescents and adults with bipolar disorder. The therapy's focus on emotion regulation skills addresses core vulnerabilities that contribute to suicidal behavior.
For individuals with comorbid substance use disorders, integrated treatment approaches that simultaneously address mood symptoms and substance use are essential. Standard psychological interventions alone show less effectiveness in this population without concurrent substance use treatment.
The BipolarLab Approach:
A Comprehensive Model for Suicide Prevention
At BipolarLab, we've developed a specialized treatment model that directly addresses the complex suicide risk factors in bipolar disorder. Our approach recognizes that bipolar disorder requires continuous, proactive management rather than episodic crisis intervention. The model follows a structured 12-step process across three critical phases: diagnostic, therapeutic, and prophylactic, with each phase building upon the previous to create a comprehensive safety net for our patients.
What distinguishes our approach is our unwavering focus on continuous prophylactic treatment—the cornerstone of suicide prevention in bipolar disorder. We understand that the periods between acute episodes are not simply "waiting periods" but crucial windows for building resilience and preventing future crises. Our model specifically avoids the use of unipolar antidepressant medications, which research has shown can paradoxically increase suicide risk in bipolar patients by triggering mixed states or rapid cycling patterns. Instead, we prioritize mood stabilization with evidence-based treatments.
Central to our suicide prevention strategy is the aggressive prevention of hypomanic, manic, and especially mixed states. These elevated or mixed mood episodes don't just represent immediate risks, they often precipitate dangerous switches into severe depressive or mixed phases where suicide risk peaks dramatically. By maintaining strict mood stabilization and preventing these destabilizing episodes, we create a protective buffer against the mood instability that drives suicidal behavior.
Our integrated approach combines pharmacological interventions with structured psychoeducation and cognitive behavioral therapy, addressing not just the mood symptoms but also the comorbid conditions, anxiety disorders, substance use, and personality issues that amplify suicide risk.
A Call for Compassion and Action
The statistics about suicide and bipolar disorder are sobering, but they're not inevitable. With proper treatment, particularly lithium therapy combined with psychological interventions many lives can be saved. The key lies in early identification, comprehensive treatment, and sustained support even during well periods of the bipolar illness.
As professionals and community members, we have the power to make a difference. Whether through supporting mental health initiatives in our workplaces, advocating for better access to care, or simply being aware and compassionate toward those struggling with mental health challenges, every action matters.
Let's commit to breaking the silence around suicide and bipolar disorder. Share this information with your network. Start conversations about mental health in your workplace. Support colleagues who may be struggling. Together, we can work toward a future where everyone with bipolar disorder receives the understanding, treatment, and support they need to live full, meaningful lives.
--
If you or someone you know is struggling with suicidal thoughts, please reach out for help immediately. Contact your local crisis hotline, emergency services, or mental health provider. Help is available, and treatment works.
Key Studies
- Christopher D Martin (2006). Ernest Hemingway: a psychological autopsy of a suicide Psychiatry. 2006 Winter;69(4):351-61. https://pubmed.ncbi.nlm.nih.gov/17326729/
- Nierenberg AA, et al. (2023). Diagnosis and Treatment of Bipolar Disorder: A Review. JAMA, 330(14):1370-1380.
- Carvalho AF, Firth J, Vieta E. (2020). Bipolar Disorder. The New England Journal of Medicine, 383(1):58-66.
- McIntyre RS, et al. (2020). Bipolar Disorders. Lancet, 396(10265):1841-1856.
- Biazus TB, et al. (2023). All-Cause and Cause-Specific Mortality Among People With Bipolar Disorder: A Large-Scale Systematic Review and Meta-Analysis. Molecular Psychiatry, 28(6):2508-2524.
- Schaffer A, et al. (2015). Epidemiology, Neurobiology and Pharmacological Interventions Related to Suicide Deaths and Suicide Attempts in Bipolar Disorder. The Australian and New Zealand Journal of Psychiatry, 49(9):785-802.
- Tondo L, Vázquez GH, Baldessarini RJ. (2021). Prevention of Suicidal Behavior in Bipolar Disorder. Bipolar Disorders, 23(1):14-23.
- Goldstein TR, et al. (2024). Dialectical Behavior Therapy for Adolescents With Bipolar Disorder: A Randomized Clinical Trial. JAMA Psychiatry, 81(1):15-24.

